Are You Sure It’s Really ADHD?
Posted on June 14, 2016 by Debra Burdick
Do you wonder if your child or teen or your client has ADHD or have they already been diagnosed with ADHD? There are many things that mimic the symptoms of ADHD and many that can increase the symptoms.
 It is impossible to make an accurate diagnosis of ADHD without all the facts. Often, clients have been referred after being diagnosed by their pediatrician who simply prescribed medication based on parent report and without examining all the factors that may contribute to symptoms of ADHD. The symptoms of ADHD may resemble and co-occur with other medical or mental health conditions, learning issues, behavior problems and vice versa.
It is impossible to make an accurate diagnosis of ADHD without all the facts. Often, clients have been referred after being diagnosed by their pediatrician who simply prescribed medication based on parent report and without examining all the factors that may contribute to symptoms of ADHD. The symptoms of ADHD may resemble and co-occur with other medical or mental health conditions, learning issues, behavior problems and vice versa.
The following is an excerpt from my book ADHD: Non-Medication Treatments and Skill for Children and Teens.
ADHD can be thought of as a result of a dysregulated brain. During the intake process look for anything that might cause the brain to be dysregulated. Children and teens may be hyperactive and distractible for any of a number of reasons.
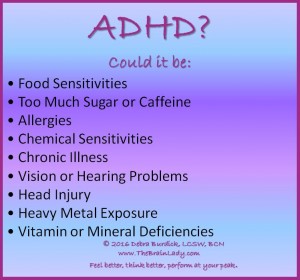
They may be suffering from:
- Food Sensitivities
- Too Much Sugar or Caffeine
- Allergies
- Chemical Sensitivities
- Chronic Illness
- Vision or Hearing Problems
- Head Injury
- Heavy Metal Exposure
- Vitamin or Mineral Deficiencies
And whether or not the person truly has ADHD, addressing these issues will contribute to overall success.
Gather all the information needed to make an accurate assessment of ADHD and to rule out other causes or contributors to the symptoms.
- Chronic Stress
- Anxiety
- Fear
- Swollen Tonsils
- A Chaotic Home Life
- A Seizure Disorder
- Trauma
- Sleep Deprivation Including Sleep Apnea
- History of trauma and Posttraumatic Stress Disorder (PTSD).
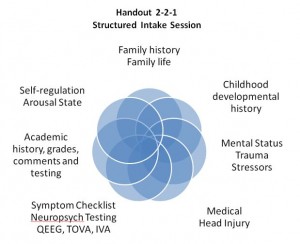
Psychological Evaluation: As with any mental health intake, do a complete assessment of mood, concentration, hyperactivity, memory, sleep, energy, appetite, medications, suicidal ideation, mental status, health and substance use. A child or teen that is sleep deprived, anxious, bipolar, learning disabled, obsessive compulsive, drug addicted, or has trouble with sensory processing may have symptoms that look like ADHD that are actually coming from these other disorders. Keep in mind that many of these are comorbid with ADHD. It is very common for the frustration of dealing with symptoms of ADHD to cause anxiety, depression and poor self-esteem. See Tool 2-8 Comorbid Disorders for more detail.
ADHD Symptom Checklist: Use the ADHD Symptom Checklist on Handout 2-1 to find out if the child or teen has the symptoms of ADHD. Ask parents (both if possible), the client if mature enough, teachers, and others involved in the client’s life to complete the checklist. See Tool 2-1 DSM-5 Diagnostic Criteria for how to use this checklist.
Does the client have trouble paying and sustaining attention? Are they able to organize their time, space, and belongings? Do they lose their homework, books, or jacket? Are they able to sit still? Are they revved up and wired? Do they interrupt others, talk all the time, say or do things without thinking? Are they tuned out, not paying attention, missing what people are saying to them? Do they try really hard but still take too long or make careless mistakes?
I often say to my client “imagine that you are sitting in class, the teacher is speaking, the student next to you is tapping their pencil, the window is open and the lawn mower is going, the door to the hall is open and the janitor walks by. What are you paying attention to?” If they have ADHD they often say “everything,” “not the teacher,” “the lawn mower.”
Observe Self-regulation and Arousal State: Observe the child or teen as they interact with you and/or their parents in session. Watch their body. Is it constantly moving? How long can they sit still? Are they fidgeting? Do they appear to be listening when you talk to them? Do they understand what you say? What’s their response time? If they are playing, how long do they stay with one toy before moving to another? Are they getting bored? Are they getting into everything?
Do they seem revved up, wired, over activated? Are they slowed, have a flat affect, not engaged, distracted? Are they complying with requests to put things away or to the rules of the session? Are they touching things that are off limits despite cues from you or parents? How long do they stay on topic? Are they telling you about one thing after another with no apparent connection between topics? How often do you have to bring them back to the topic you are discussing? Are they zoned out, not paying attention nor responding? Are they interrupting when you or their parents are talking? Are they demanding attention? What is their level of self-awareness, if any?
Phew! You will learn a lot about the child’s ability to regulate their arousal state just by watching them. If they are over- aroused they may have the hyperactive/impulsive type of ADHD. If they are under-activated they may have the inattentive type. Additionally, you will discover how they comply with adult requests, who is in charge in this family (often not the parents), what their frustration tolerance is, whether they are comfortable in their own skin or anxious, depressed, or oppositional.
This is just one important piece of the diagnostic puzzle.
Family History: There is a genetic link for ADHD which makes it more likely to have ADHD if a family member has it. During the intake process ask about family history of symptoms similar to those the client experiences (Wolraich, 2006). Keep in mind that a grandparent or parent might not have been diagnosed with ADHD, but the family may be well aware if they exhibited symptoms of ADHD. ADHD is not 100% inheritable. Therefore, having a family member with ADHD does not necessarily mean your client has it, but makes it much more likely. Also, not having a family history of ADHD does not rule it out for your client.
Developmental History: Ask about any issues with the mother’s pregnancy, the birth, and early medical issues. Did the child meet normal developmental milestones such as crawling, walking, talking and toilet training? Were there any particular problems the parent can remember? Was there an event that occurred that seemed to derail development or reverse it? A developing brain can be impacted by many things that often go unnoticed. Is there any history of neglect or abuse? Is there any evidence of reactive attachment disorder?
Medical History, Mimics and Contributors: Were there any medical issues during the pregnancy, at birth, and/or up until now? Ask about illnesses, ear infections, injuries, accidents, sleep, medications, allergies, food sensitivities and genetic issues. See Tool 2-7 for things that can mimic and contribute to ADHD, Chapter 21 Assess and Improve Sleep for more information about sleep and ADHD and Chapter 19 Common Sensitivities for help with identifying food sensitivities.
Head Injury: Head injury is often overlooked or minimized. A person does not have to have a traumatic brain injury (TBI) to experience symptoms that look like ADHD symptoms but that are really caused by a head injury sometimes sustained years ago. The brain can sustain damage even from a ‘bump’ on the head. The brain floats in fluid and when the head is hit the brain bounces up against the skull on the opposite side of the head and then back again. There is evidence that brain injury can be cumulative. This is showing up in teenagers who hit their head while playing football.
Children and teens often hit their heads and seem to be okay afterward. Even if a CT scan or an MRI indicates no problem, the functioning of the brain can be impacted for years afterward. The symptoms of a head injury can be similar to ADHD symptoms, but the treatment may differ.
When talking with your client or their caregiver, be sure to ask about any history of hitting their head no matter how insignificant it may have seemed at the time. Did they get a bump or a bruise, lose consciousness, need stitches or receive a concussion diagnosis? See Tool 2-3 QEEG for a case example of a seven-year-old girl initially diagnosed with ADHD, who had a concussion at age two, and its impact showed up on a quantitative EEG (QEEG) five years later.
Sensory Integration: If a client has a sensory processing or modulation disorder they have difficulty regulating and organizing responses to sensory input from the environment and their body. This can impact their motor function, emotional state, arousal and attention. The overlap of symptoms of Sensory Modulation Disorder (SMD) and ADHD makes it difficult to differentiate between the two. A client who appears wired or distracted may look like they have ADHD but may actually be having trouble processing sensory input. (Miller, 2012), (Mangeot et al, 2001) See Tool 14-1 Sensory Integration Therapy for more detail.
Trauma: A child or teen that has experienced trauma may exhibit symptoms that look like ADHD as the trauma can dysregulate the brain in specific ways. Trauma can be a result of verbal, emotional or physical abuse, injury, illness, neglect, or witnessing or experiencing something that felt traumatic to the child. Look for any history of trauma and rule out Posttraumatic Stress Disorder (PTSD).
Academic: How is this child performing in school? Children with ADHD often do very well in the first few grades but then start to struggle as the work gets harder and more demanding, usually by third grade. Learning disabilities may mimic the symptoms of ADHD and may be present in addition to ADHD. It is important
to make sure the child receives all the necessary testing in school to assess this. Look at the comments on their report card. If a child or teen has ADHD the comments will likely contain statements such as: trouble sitting still; difficulty staying on task; not working up to potential; talks out of turn; fails to raise his hand to speak; annoys other students who are trying to work; easily distracted; loses his homework, books, pencils; very social; needs constant attention and cueing; daydreams a lot. The comments usually give a more accurate picture of the symptoms of ADHD than the grades.
Family Life: Explore the dynamics of this client’s family life. How is the family functioning? Is there a lot of conflict, anger, lack of structure, or chaos? Where does this child or teen fit into the family? How are they treated by parents and siblings? What words do the parents and siblings use to describe them? What is the birth order of this child? How do they get along with their parents and siblings? What expectations do the parents have of this child or teen? Are the client’s symptoms stemming from family issues and not truly ADHD? Is there appropriate structure in place throughout the day? Family life can have a significant impact on the child or teen’s functioning and ADHD symptoms can have also have a significant impact on the functioning of the family.
Social: ADHD symptoms can interfere with a client’s ability to have good relationships with parents, peers, teachers and others. Some clients become alienated from peers due to their impulsivity, hyperactivity, less developed social skills, and behaviors that annoy potential friends. Even when children with ADHD have friends in elementary school, these friends may fall away as they get older and more mature. Some friends may no longer have the patience to deal with the annoying behaviors. On the other hand, some children and teens with ADHD are very successful socially and have lots of friends.
Find out how the client is doing socially. Do they have friends? Ask them to name a few. Do they ever connect with them outside of school? Who do they sit with at lunch? How do they get along with the neighborhood kids? Are they wishing for more friends? Do they struggle socially and not understand why? Do they have self-awareness about how their behaviors may push others away?
Nutrition: Find out what this client is eating. What does their daily diet consist of? Nutrition can have a significant impact on the brain of a child or teen with ADHD. Look for excessive sugar and caffeine consumption. How often do they eat? What proteins, fruits, vegetables and whole grains do they include in their diet? Do any foods bother them or make their symptoms worse? See Section IX Nutrition for the ADHD Brain for specific nutritional information and guidance for ADHD.
Stressors: What types of stressors are present for this client? Are they under a lot of pressure at school? Are they behind in their work? Are they failing courses? What pressures exist at home? Are parents angry with them? Is anxiety about performance or fear of failure a factor? Look at how this client is functioning in his
environment. Do their symptoms cause stress for them? Perhaps there are accommodations that might remove some of the stress at school. See Chapter 22 School and ADHD for common accommodations that might be helpful.
Previous Testing: Get copies of all previous testing that has been done in school and elsewhere. This may include psychological testing, IQ testing, testing for learning disabilities, and assessments for ADHD. Review the results to see if they indicate that ADHD may be present. Also look for indications of anxiety, depression, low self-esteem, bipolar disorder and oppositional defiant disorder.
Records from Previous Treatment: If possible, get a “Release of Information” form signed to talk with the referral source and gather as much information verbally and via treatment records as possible. Get discharge records from previous therapists or communicate with other therapists that are still involved.
Neuropsychological and Academic Testing: There are a number of excellent tests that measure concentration, intelligence, short term and long term memory, response time, impulse control and more. Neuropsychological testing can isolate the area of the brain that is underperforming and can aid in the diagnosis of ADHD. Neuropsychologists and school psychologists are the professionals who typically administer these tests. Each neuropsychologist or school tends to use their favorite set of tests.
INTEGRATION: Now that you have gathered information about all the pieces of the diagnostic puzzle, review everything and ask yourself “are the symptoms truly coming from ADHD or something else, or perhaps both?”
I would love to hear your personal experiences with this topic.
Categories: ADHD, Articles, Neurofeedback
Tags: ADHD, ADHD Diagnosis, adhd treatment




No comments yet. You should be kind and add one!
The comments are closed.