PTSD
When an individual who has been exposed to a traumatic event develops anxiety symptoms, re-experiencing of the event, and avoidance of stimuli related to the event lasting more than four weeks, they may be suffering from PTSD. This diagnosis was originally devised for veterans returning from war zones. It is important to realize that an event that feels traumatic to one person may not feel traumatic to another.
 Diagnostic criteria for 309.81 Posttraumatic Stress Disorder
Diagnostic criteria for 309.81 Posttraumatic Stress Disorder
- The person has been exposed to a traumatic event in which both of the following were present:
- the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others
- the person’s response involved intense fear, helplessness, or horror. Note: In children, this may be expressed instead by disorganized or agitated behavior
- The traumatic event is persistently re-experienced in one (or more) of the following ways:
- Recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions. Note: In young children, repetitive play may occur in which themes or aspects of the trauma are expressed.
- Recurrent distressing dreams of the event. Note: In children, there may be frightening dreams without recognizable content.
- Acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur on awakening or when intoxicated). Note: In young children, trauma-specific reenactment may occur.
- Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
- Physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
- Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three (or more) of the following:
- Efforts to avoid thoughts, feelings, or conversations associated with the trauma
- Efforts to avoid activities, places, or people that arouse recollections of the trauma
- Inability to recall an important aspect of the trauma
- Markedly diminished interest or participation in significant activities
- Feeling of detachment or estrangement from others
- Restricted range of affect (e.g., unable to have loving feelings)
- Sense of a foreshortened future (e.g., does not expect to have a career, marriage, children, or a normal life span)
- Persistent symptoms of increased arousal (not present before the trauma), as indicated by two (or more) of the following:
- Difficulty falling or staying asleep
- Irritability or outbursts of anger
- Difficulty concentrating
- Hypervigilance
- Exaggerated startle response
- Duration of the disturbance (symptoms in Criteria B, C, and D) is more than 1 month.
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.Specify if:Acute: if duration of symptoms is less than 3 months
Chronic: if duration of symptoms is 3 months or more
Specify if:
With Delayed Onset: if onset of symptoms is at least 6 months after the stressor
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, Copyright 2000 American Psychiatric Association
TREATMENT
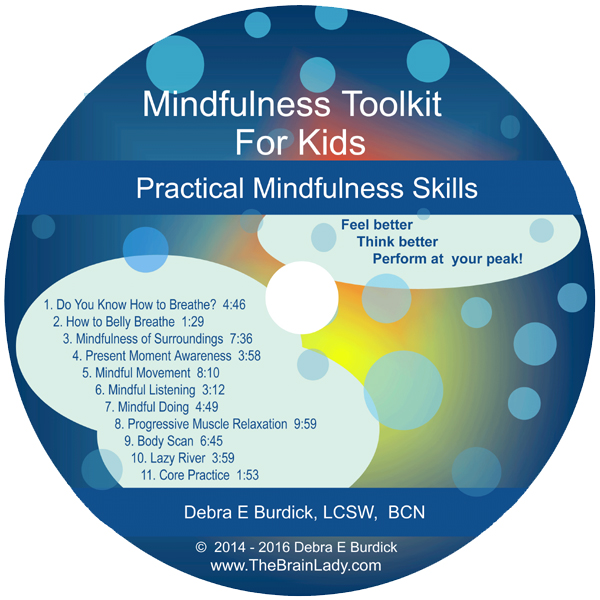
Many options exist for treating PTSD. We combine psychotherapy, Mindfulness, Neurofeedback, and Havening (a technique for treating trauma developed and research by Ronald Ruden) to treat PTSD and reduce its impact on the life of the client. The traumatic memory gets stored (often as an implicit memory) during the trauma and often gets reactivated unconsciously thereby causing the event to be re-experienced as if it is happening again in the present. The goal of treatment is to deactivate the power of these traumatic memories and to reprogram the neuronal pathways that may have become stuck in negative patterns.
One of my clients came in for treatment twenty four years after he was stationed in a war zone. He was suffering from flashbacks of the horrible things he had experienced as an American soldier in the war. He was using alcohol to medicate his anxiety and avoid the horrible memories. I treated him with a combination of psychotherapy and Neurofeedback and soon he was able to go to sleep without placing a gun under his pillow as he had done for 24 years, and he was able to sleep soundly through the night. His alcohol use diminished and then stopped. His energy returned and he was no longer haunted by the horrible flashbacks.
A woman came in for treatment of chronic and debilitating pain. I discovered during the intake session that she had experienced physical and emotional abuse as a child as well as a horseback riding accident. I combined psychotherapy, mindfulness, and Neurofeedback which resulted in a significant reduction in pain and stabilizing of mood. In fact her pain/spine doctor started referring many of his patients to me as he had never seen such improvements in long standing pain. It is not uncommon to find that people who have chronic illness or pain have some trauma history.
Caution: The information presented here is for your reference only and should not be used to diagnose or treat any condition. It is not intended to substitute for the advice of you or your child’s medical doctor or mental health professional.
PLEASE NOTE: As of December 31, 2014 Deb has retired from her private practice and is no longer accepting new clients so that she can concentrate on writing and teaching. The above is for historical/informational purposes only.